This post is devoted to developing an EHR solution from scratch. However, we know that a considerable number of healthcare providers prefer to use time-tested EHR systems via EHR integration APIs. If you’re among them, you might be interested in integrating your software with an EHR platform. In this case, be prepared to face some of the challenges we’ve experienced while integrating with EHR products from vendors including Greenway Health, Allscripts, and Cerner.
EHR integration pitfalls
Working with HL7 standards
HL7 v2, HL7 v3, and FHIR are the main healthcare data-sharing standards. Many ready-made EHR systems follow HL7 specifications to format messages. Each of the three HL7 standards is peculiar in its use.
For example, the HL7 v2 standard doesn’t provide structure to messages, which increases development and maintenance costs. Furthermore, even the slightest changes in the system may lead to its not processing data. Unlike FHIR, which is based on HTTP and web technologies, HL7 v2 and HL7 v3 usually require creating additional software to integrate with an EHR system.
Working with medical data dictionaries
EHRs use different systems of collateral information support (collections of medical terms like SNOMED CT, databases like LOINC, classification systems like ICD). By integrating with these systems, a doctor can choose a diagnosis and medications in a provider-facing EHR system.
These systems are hard to work with, as they provide large amounts of unstructured data. You need to find a solution to parsing, structuring, visualizing, and storing such data. At Yalantis, we have developed approaches to working with this kind of data depending on our clients’ business needs and use cases. Our expertise stretches from ensuring display of diagnosis by working with diagnosis classifiers to enabling interoperability among several EHRs used by a clinic.
EHR vendor certification requirements
For your organization to be given access to real EHR data, the EHR vendor must make sure you can properly work with the data and with the system in general. That’s why you have to get your software certified. Each EHR vendor has its own software certification requirements.
In addition, certain functionality requires certification from dedicated government and non-government institutions. These can be Health IT certifications for processing and working with Continuity of Care Documents outside of EHR software (such as for displaying encounters in patient-facing applications).
A software development partner that provides EHR integration services and is experienced in EHR integration and development will help you overcome the above-mentioned challenges and create an EHR solution from scratch. There are good reasons to do this.
Is an electronic health record (EHR) system a magic pill?
NEED A SECURE AND EASY-TO-USE EHR SYSTEM?
We deliver EHR development and integration services to streamline your medical workflow
Not necessarily. Electronic health records are meant to improve healthcare processes and serve patients. So why do clinicians give this technology an “F” rating for usability in a 2019 study by Yale University? For context, look at how participants in other studies rank different programs and devices in terms of usability:
A — Google search engine
B — Microwave ovens, ATMs, and Amazon
C — Microsoft Word, DVRs, and GPS devices
F — Microsoft Excel (due to its steep learning curve)
In the study conducted by Yale, healthcare professionals gave EHR solutions a usability score of 45, which is even less than Excel’s 57. The same Yale-led study discovered that EHRs are also contributing to doctors’ burnout. What’s the reason for these depressing results?
The US HITECH Act of 2009 was well-intentioned, but it pushed healthcare providers to adopt unknown and complicated technology as quickly as possible. In trying to become digitized, the healthcare industry is increasingly experiencing security and workflow issues, leading to frustrated clinicians and dissatisfied healthcare consumers.
But giving up on ineffective, buggy, and clumsy software you’ve almost gotten used to means having to walk the road of complex new implementations once again. And while adopting new software does require an investment of time and money, it doesn’t guarantee a positive outcome. This is why C-level managers of healthcare enterprises hesitate to change their EHR systems but still are interested in how to build an EHR solution.
If you realize that your current EHR is blocking your practice from growing and prospering, this article will show you how you can break the vicious cycle and implement an effective EHR solution.

What irritates clinicians about their EHR solutions
A study by the University of New Mexico found that the design of clinical processes and clinical culture — both of which are directly related to the use of EHRs — contribute to nearly 40 percent of the total stress experienced by healthcare specialists. Let’s check out what EHR complexities lead to clinician burnout.
Time-consuming operations
The University of New Mexico study points out that doctors spend one to two hours on EHRs and other deskwork for every hour spent with patients and spend an extra one to two hours of personal time on EHR-related operations on a daily basis. No wonder they do, as scheduling a computed tomography scan through an EHR might take 45 minutes.
Moreover, EHRs — often, even different EHRs provided by the same vendor — are not interoperable between different facilities. Consequently, a patient’s tests may be repeated as many times as a patient goes to a new facility.
EHRs are prone to errors
The problem of patient misidentification is increasingly evident. Take, for example, an incident that happened in 2019 at Virtua Our Lady of Lourdes Hospital in New Jersey, when a patient received a kidney transplant that was destined for another patient of the same name and age. Luckily, the intended recipient obtained a transplant a few days later and both patients are okay, but many similar incidents have been caused by the use of EHRs.
EHRs are difficult to use
EHRs are complicated and feature-packed. Customizing an EHR requires lots of manual work and may not be fully successful due to the system’s rigidity. The need to be tech-savvy and ready to deal with puzzling interfaces is driving some clinicians right out of the profession, as a mistake might cost a life. Additionally, EHRs keep requiring excessive mouse clicks and pagination to insert information during appointments, deflecting attention from patients.
Let’s see how these issues manifest themselves in the most used and seemingly reliable EHR software.
What’s wrong with the leading EHR software systems?
Cerner and Epic are undisputed leaders in the US EHR market. According to a report by KLAS, they hold 54 percent of the US acute care hospital market, with Epic having 28 percent and Cerner 26 percent of the market share.
These vendors provide comprehensive and expensive EHR systems, multi-year contracts for which usually cost millions or even billions of dollars. Adopting Cerner or Epic software might take from six months to more than a year, not counting the time needed by employees to adapt to the new system. When choosing either of these products, healthcare organizations fairly expect state-of-the-art software and service. But along with sophisticated functionality and extensive software integration capabilities, you may encounter the following issues.
Barriers to caring for and serving healthcare consumers
Here are examples of how EHR solutions might cause harm to patients’ health and a hospital’s operations, leading to significant financial and reputational damage.
Epic. In 2015, suspecting that a patient was suffering from meningitis, a physician at the Saint John’s Health Center in Los Angeles carried out a spinal tap. Next, an infectious disease specialist ordered a critical lab test in the Epic EHR. The order was placed successfully according to the user interface, but as it turned out later, it wasn’t forwarded to the lab. The patient’s test results were delayed a few days, resulting in irrevocable brain damage from herpes encephalitis. The error might have been caused by the Epic EHR not completely “interfacing” with the lab’s system. Epic claimed it was the hospital specialist’s fault, as they allegedly used the wrong button and it was the hospital who had configured the interface with the lab. But three years later, Epic paid $1 million to settle the suit. The medical facility and its two healthcare specialists paid a total of $7.5 million, and one case against a third specialist is pending trial.
Cerner. In 2017, the Glen Falls Hospital in New York experienced constant issues with their billing system. This resulted in $54 million in uncollected bills. Of these uncollected bills, $38 million were directly related to the Cerner EHR system used by the hospital. Hospital staff said that bills weren’t sent out of the facility for several months due to issues with the Cerner EHR system. Other hospitals, like the Western Missouri Medical Center, have also experienced serious financial losses caused by the Cerner EHR billing system.
Usability issues
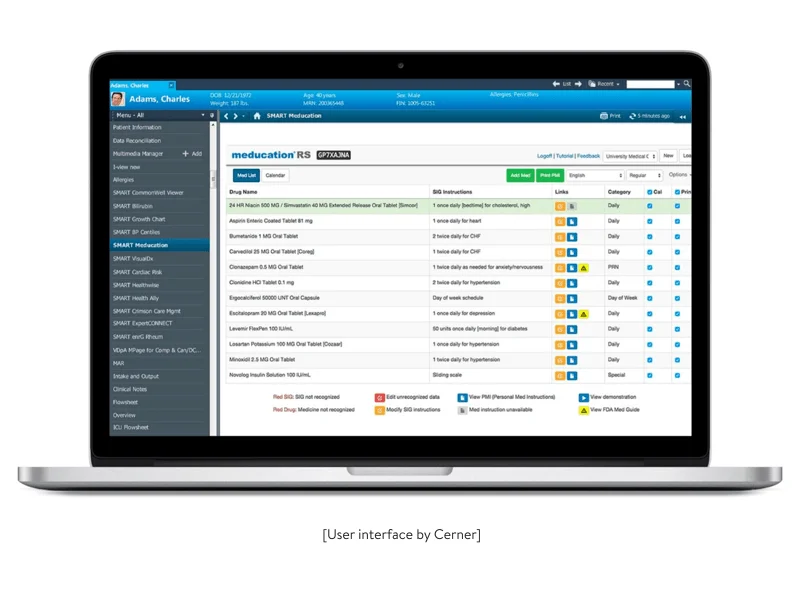
Cerner provides an aesthetically pleasing graphical user interface, but it isn’t easy to navigate. Lots of users complain about long and repetitive workflows to perform even simple tasks. Employees will require comprehensive training before they feel comfortable using the Cerner system.
When it comes to Epic, many doctors have written about its overwhelming complexity: the dashboard is overloaded with buttons, switches, lights, and levers. According to a post published by The New York Times and written by Emily Silverman, M.D., the Epic EHR makes sudden and premature requests, mid-documentation, to “assign” patients diagnoses from a list of extremely specific options.
Considering clinicians as task performers rather than humans
In the post just mentioned, Dr. Silverman shares impressions of using the Epic EHR system. Dr. Silverman recognizes the lack of supportive components in the system, saying that staff receive ruthless daily reminders about tasks they haven’t performed with no praise for what has been accomplished. This makes physicians feel constantly deficient.
Besides Epic and Cerner, there are countless other ready-made EHR solutions out there. But they receive even more user complaints. It’s no wonder the level of EHR dissatisfaction among clinicians is so high. So what’s the way out?
The answer is to build a custom EHR solution that incorporates all the best practices you appreciate in leading off-the-shelf software and is tailored to the specific needs of your practice.
Why develop a custom EHR?
Check out the most obvious reasons for custom EHR development.
Implement all the features you need — and nothing you don’t
A modern EHR might contain features for chronic disease management, behavioral health support, e-prescribing, and surgery preparation. It might even provide drug diversion tools to ensure proper prescribing methods.
Developing a custom EHR empowers you to pick the features needed by your practice. At the same time, you don’t have to implement unnecessary functionality that will confuse your employees and cause them to get lost in a mindblowing assortment of options.
Implement only the integrations you need
Let’s say you currently have two different EHRs: one for your hospital and the other for your private practice. You have two interfaces, but in addition, there are 40 different programs that must exchange data with these systems and communicate with each other. A software development partner can help you implement a single EHR that incorporates all your practice and hospital processes into a single interface.
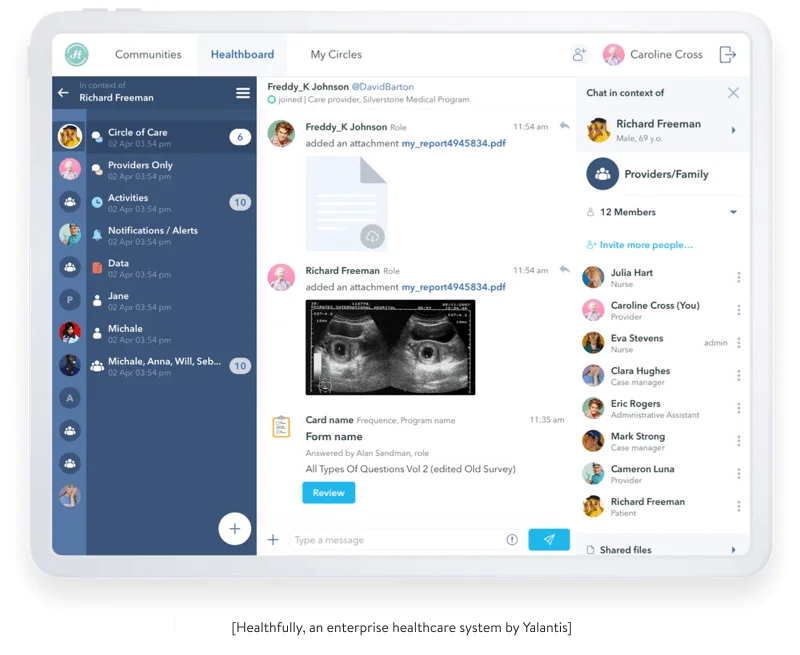
While working on Healthfully, an enterprise eHealth system, we ensured integrations with EHR, HL7, telemedicine, payment, and WebRTC solutions. Such an approach helps us smoothly integrate healthcare solutions with numerous EHR systems, such as Epic, Cerner, Athenahealth, and other systems. Some of the solutions we needed to integrate with were poorly documented legacy systems, but we ensured system integrity despite the variety of tech stacks we used.
Timely improvements and quick support
According to some users’ complaints, Epic customer support is not very responsive to improvement requests regarding simple tasks that could be performed more easily by adding a button or checkbox in specific areas. Downtime for the service might also be problematic if maintenance needs to be done during work hours.
When developing a customizable software solution with a development partner, you can expect thorough initial research and testing of features by end users along with the collection, analysis, and implementation of improvement requests.
When building Healthfully, we established a process for collecting feedback regarding features under test and providing prompt fixes, as the functionality we were developing was urgent for our client.
Training end users
Your EHR software development partner can also offer to train your staff and ensure further support and maintenance. And in case you have requirements for urgent new functionality, your partner will be there for you.
Due to the COVID-19 outbreak, Healthfully needed back-to-work, back-to-school, and telehealth functionality. We implemented all these features within two weeks.
Learn how we built a SaaS appointment scheduling system with an EHR module
READ THE CASE STUDYCritical elements to consider before starting EHR solution development
You must first determine what type of EHR system you need:
- Inpatient EHRs are used mostly in clinics and hospitals
- Outpatient (or ambulatory) EHRs are used for monitoring patients who don’t require inpatient care
The development of each type of system calls for special attention to its peculiarities.
What to equip inpatient EHRs with
Inpatient EHRs are more commonly utilized in healthcare facilities, and their development and deployment are more difficult. A hospital is a complex organization with multiple departments, each with its own set of operational requirements — all of which must be considered during development.
An inpatient EHR system must be capable of supplying vital data to medical staff and patients in any format, be it a simple spreadsheet with test results or radiographs. Furthermore, throughout cooperative therapy, all departments must work together.
These are some features we advise for your EHR solution to streamline the treatment process:
- A single patient database where a physician fills in basic information about a patient to prevent future mistakes; specialists from other departments must only enter information relevant to their field of work
- As part of a personal data protection program, medical employees (doctors, nurses, and hospice workers) should be given several levels of access permissions
- Fast access to patient information for specialists from other medical facilities in the event of an emergency transportation request, as well as to information on doctors’ orders for admitting a patient to inpatient care
What to ensure when creating an outpatient EHR solution
Outpatient EHR solutions must be able to accompany patients outside of healthcare facilities in a comfortable manner. Ambulatory patients have more freedom of movement and are more responsible for their own health and treatment.
An outpatient EHR provider must assess the unique needs of such patients and assist in the creation of a strong patient-to-doctor communication channel that allows a doctor to stay informed about a patient’s condition.
What to include in an outpatient EHR system:
- A user-friendly solution with comprehensible and easy to use telemedicine functionality for strengthening patient–physician communication
- Periodic information gathering from wearables (if a patient uses them)
- Both a doctor and a patient must receive a notification to contact each other under special circumstances, such as missing an appointment
- A tracker for taking medicine in the form of an electronic medicine log where a doctor can keep track of the right dosage and medicaments
- A database of pharmacies and labs throughout the city or state a patient resides in; whereas patients in a hospital are limited to the hospital’s pharmacy and labs, ambulatory patients’ options are not constrained
To ensure both types of treatment in a single unit, a medical facility can create a unified EHR solution with inpatient and outpatient monitoring features. Developing such a solution will be more challenging and will require an experienced healthcare software provider that will be able to take into consideration the peculiarities of both systems.
Go further with functionality for behavioral health
A behavioral health EHR system is another type to contemplate given the heightened concern about mental and physical health. Such a system can be an independent solution for monitoring patients who are prone to behavioral health problems or part of a single across-the-board EHR system that accommodates the requisite features.
Behavioral health is broader than mental health and physical health, which are subsets of it. Behavioral health embraces behavioral patterns, positive and negative, that may or may not lead to mental diseases as well as physical health issues.
A behavioral health system necessitates a set of features that will aid in the development of stronger trust between a doctor and a patient as well as keep a doctor informed of any changes in a patient’s behavior in order to predict and prevent the onset of diseases.
Behavioral EHR functionality may include:
- An observation log of everything patients experience, including their moods, feelings, and thoughts
- Information in the form of guides or advice on how to get through a crisis if there is no way to contact a doctor
- Telemedicine solutions for contacting a doctor or volunteers who can always consult or just listen to a patient
- Communities of interest so patients can share their experiences and find support
- Periodic quizzes and surveys to help a doctor understand the general background of patients’ conditions and ups and downs in their treatment
- Basic meditation and exercise sets to help patients relax and direct their energy on the right track
EHR solutions are unquestionably powerful in terms of functionality and benefits. Any provider of such a system, however, should keep in mind the certification process that must be completed before the system can begin to operate.
Certify your EHR solution
Governments and independent commissions have particular requirements that your EHR solution must meet. That’s why, when choosing a healthcare software provider, you should determine whether a company has any experience going through:
-
The ONС IT Health Certification Program to show that your EHR complies with government-mandated criteria
-
The Certification Commission for Health Information Technology (CCHIT) to show that your EHR has been audited for functionality, compatibility with other health IT, and security
Yalantis has experience obtaining ONC Certification for software we build and can help your medical facility create an all-in-one EHR solution.
After clarifying reasons for building EHRs and identifying features that different systems require, let’s explore how to build an EHR system.
EHR solution development: where to start?
These three steps will help you overcome your most burning healthcare business challenges with an EHR app.
Step 1: Define your strategic goal. For example, if your goal is to reduce patient turnaround times, you might consider integrating an appointment scheduling feature, video chat, etc.
Step 2: Talk to your users about their needs. Your clinical staff, customers, and even insurance providers can provide you with valuable insights into how to refine your software and make it more patient- and hospital-oriented.
Step 3: Document your requirements. Once you’ve defined your strategic goals and your users’ needs, you can transform them into business requirements, based on which you can prepare a functional specification. Your technology partner can help you with this.
Let’s see what needs and objectives your EHR app should cover.
Minimizing paperwork and optimizing data entry
While doctors can obtain some information directly from different sources, they still have to enter or upload data to an EHR. That’s where human errors might occur. Sometimes, EHRs even contribute to the appearance of errors.
For example, some EHR systems remove the decimal point when a provider types in a medication dose. If a doctor were to type in an order for 2.5 milligrams of medication in such a system, this would actually be processed by the EHR as 25 milligrams. This error could lead to an overdose. Developers must avoid such inconsistencies.
Here’s how an EHR can minimize the possibility of errors:
Data entry
There might be cases when a patient is weighed in pounds but the patient data has to be inserted into the EHR solution in kilograms. To ensure accuracy, units must be clear in the interface. The general principle of the data entry process is simplicity and data consistency.
Precise editing
Copying and pasting is an important functionality that cuts time and cognitive burden for healthcare specialists. However, poorly implemented copy-paste functionality can pose risks to healthcare consumers. Users might fail to check and edit data, as an EHR doesn’t help them do that. To enable users to spot inaccurate information, an EHR might ensure:
Automatic data updates. An EHR may automatically update notes with current vital signs and test results. Displaying the name of the author on all notes can help doctors see whether a recent note has been updated from a previous version. The author’s name can remain the same if the note is copied with no revisions but change if another doctor reviews and edits it.
Сentralized data matching system. A centralized data matching system automates record de-duplication and data integrity. An efficient enterprise master patient index (EMPI) is essential in providing a smooth data flow from provider to provider. EMPIs that use location intelligence and geocoding to check addresses help healthcare providers standardize and authenticate addresses in real time. This helps to avoid risks related to duplicate records and detect fraud.

Searchability, advanced decision support, and reporting
To let your users build queries for both structured and unstructured data, you need to use a search engine that can handle unstructured documents, offers a flexible API, and is highly configurable and scalable — Elasticsearch, for example.
It’s also advisable to present the results of treatment and whole treatment processes in progress dashboards, giving information in an easy-to-understand format. This way, you’ll make it easier for doctors to make informed decisions about a patient’s diagnosis, current health condition, and treatment plan.
Your product should be equipped with a powerful analytics and reporting framework capable of generating all types of medical reports to help you meet your business goals and provide the best service. Bear in mind that the types of reports your system needs to generate will depend on your requirements.
Improving customer engagement and providing transparency
When wisely implemented, patient engagement features benefit patients by putting them in control of their health and benefit clinicians by giving them more time to focus on patient care. A patient portal can lead to a high level of patient engagement. Let’s see what a helpful patient portal should include to improve the user experience and increase patient loyalty.
Appointment scheduling
Online appointment scheduling not only greatly increases patient satisfaction but also saves time for your staff, letting them spend less time on phone calls and focus on more important tasks. What’s more, by integrating your app with push notifications or simple SMS reminders, you can significantly reduce the number of no-shows, which is bound to increase your revenue.
Health risk assessment (HRA) tool
Preventing illness is better than curing it. Allow your patients to enter data about their state of health using questionnaires or chatbot functionality. An HRA tool allows your patients to prevent severe consequences of their lifestyles, mitigate genetic predispositions to certain diseases, and minimize the possibility of contracting infections. Using HRA functionality, doctors can detect potential symptoms and take appropriate measures to prevent serious illnesses.
Access to lab results and medication records
Your lab integration module should automatically upload lab results to the EHR system and make them available to both doctors and patients. What’s more, it should show explanatory notes next to each result. This will help doctors and patients quickly understand which results are within and outside the norm.
Enabling adequate data protection
The HIPAA Security Rule requires all healthcare providers to take physical, administrative, and technological measures to protect private information. For EHR systems, this means providing access controls, data encryption, audit controls, activity logs, etc.
While working on Healthfully, we ensured its HIPAA compliance. We also ensured that users only had access to appropriate data layers in the app as part of the app’s compliance with FDA requirements for medical app data security.
In addition, we made sure the app’s control system allows users to access their information both on the web and in the mobile app via a secure HTTPS connection. To ensure the smooth operation of the access control system, we created a separate module based on the open source CanCan component. Other modules request data from this module to understand what level of access users have.
Improving interoperability
There are two keys to effective EHR interoperability between healthcare providers:
- Creating and promoting an open application programming interface (API) that will allow for the sharing of unified medical records. Ideally, this API should be easy for medical workers to set up and configure.
- Following a unified standard for exchanging information between healthcare providers. By following established standards such as fast healthcare interoperability resources (FHIR), developers help healthcare organizations speed up the adoption of app-based solutions that support data interoperability.
A few more tips for creating an EHR system
Here are some tips on how you can guarantee the highest level of usability for your medical personnel and patients.
Minimize the number of clicks required. Unfortunately, most EHRs require users to make excessive clicks.
Consider doctors as humans. Try to find a human tone of voice. If there’s no real emergency, make the interface colors and symbols neutral, even calm. Notifications regarding a patient’s death should provide empathy. What Epic calls “deficiencies” and “delinquencies” might be named “incomplete tasks.” Periodic encouragement with messages like “thank you for all your hard work” will inspire and support users.
Consider integration with wearables. To monitor patients’ vitals, manage chronic diseases, and support post-surgical observations, you can parse data directly from wearable devices or health applications such as Google Fit and Apple Health through these medical software platforms’ native APIs.
Now you know how to create an electronic health record system. As you can see, a custom EHR can bring a lot of benefits to your healthcare business: fewer disparities and errors in medical records, better engagement with patients and their families, improved decision-making and care coordination, and increased security for your patients’ data. But before deciding on a software development partner, make sure they’re highly experienced in building complex high-quality projects, creating service-oriented architectures, implementing electronic medical record systems, and providing cost-efficient services.
Want to build EHR software? Yalantis, which has been ranked one of the top software outsourcing companies in Ukraine by Clutch, would be a great choice. Tell us about your most burning pain related to your EMR/EHR software solutions and we’ll help you treat it with a custom web or mobile medical app.
Rate this article
2.8/5.0
based on 11 reviews