The number of virtual healthcare visits has soared. Before the pandemic, only one percent of doctors’ visits were held virtually in the US. But in just the first month of the COVID-19 pandemic, that number jumped to nearly 50 percent according to the ATA, an organization that works on improving telehealth and that has analyzed Medicare claims data.
This trend will affect how healthcare services are delivered in a post-COVID world. While the rate of telehealth use is no longer increasing as quickly as it was in spring 2020, it remains much higher than before the pandemic and shows no signs of decreasing.
What helps healthcare providers quickly adopt telehealth services?
The US federal government has temporarily relaxed previous telehealth restrictions during the COVID-19 crisis to ensure easier provision of telehealth services.
Some of these temporary changes allow providers to:
- Provide telehealth services to Medicare patients outside of designated rural areas and even across state borders
- Serve not only established but also new Medicare patients via telehealth
- Offer any healthcare services via telehealth at the provider’s discretion
- Charge for telemedicine visits (both video and audio-only) at the same rate as in-person visits
- Use widely available communication solutions such as FaceTime, Facebook Messenger, Google Hangouts, Zoom, and Skype, even if the solution doesn’t fully comply with HIPAA requirements
Questions are emerging among healthcare providers as to the reasonableness of this last provision, however, and for good reason.
Enhance remote care with telehealth software
We develop feature-rich telehealth solutions to help medical practices serve more patients
What’s wrong with existing communication and telehealth solutions?
First, the security of popular communication solutions leaves something to be desired. Take Zoom, for instance. Recently, the Federal Trade Commission (FTC) accused Zoom of misleading users and engaging in a string of delusory and unfair practices related to its security. The FTC pointed out fake end-to-end encryption and mentioned the software that Zoom installed on Macs without authorization in 2018 and 2019.
Second, common communication solutions don’t provide adequate APIs. This means you can’t implement additional functionality when using them, which is essential for full-fledged telehealth software systems. Such functionality might handle patient profiles, payment processing, notifications, appointment scheduling, reporting, and remote patient monitoring. Having such functionality in a web-based telemedicine system is possible only when you choose software specifically tailored to telehealth.
Off-the-shelf telehealth software
There are a number of ready-made telehealth solutions on the market. Vectera, eVisit, and Doxy.me are some of the most prominent telemedicine solution providers, as they give doctors a quick way of delivering HIPAA-compliant telehealth services.
But in the long run, these are not optimal solutions. Here’s why:
Price. Telehealth patient communication platforms will charge you for a license or subscription, but be prepared to pay extra for essential features. With Doxy.me, for example, to get a monthly usage report or add multiple participants to a call, you have to choose the most expensive Clinic plan.
Poor customizability and feature sets. With existing platforms, there’s not enough flexibility to quickly adjust your software to fit your existing workflow, and some features you need might be unavailable. For instance, Vectera doesn’t provide e-prescribing. The eVisit feature set is even poorer: the platform doesn’t offer appointment reminders, billing, or even appointment scheduling. Moreover, if you use any SaaS solution, you can’t store data on your own servers, which is sometimes critical for a medical practice.
Unreliable support. During emergencies like the COVID-19 pandemic, a telehealth platform’s support team might be too busy to be reached, and there may be nobody to help you if the service goes down. That’s what happened to Doxy.me customers in April 2020 during the spring coronavirus peak.

Why telehealth is here to stay
COVID-19 triggered the use of telehealth services. Doctors, patients, and medical practices tried this digital health technology, and it turned out that health virtual healthcare visits can be much more convenient than in-person visits. Moreover, it seems that many things doctors initially thought they could only provide during an in-person visit might be successfully provided online. The positive experience with telehealth services and unease with in-person visits caused by the pandemic are leading to increasing demand for telehealth services from all parties.
Patients are supporting the virtual revolution
Consumers wanted telehealth long before COVID-19. The Virtual Visits Consumer Choice Survey 2017, for which Advisory Board surveyed more than 5,000 patients across the US, discovered that 77 percent of those patients wanted to participate in virtual care and 19 percent had already done so. Since then, many things have changed:
- A 2020 doctor.com report demonstrated that the rate of patient adoption of telehealth was up 33 percent over 2019.
- According to McKinsey, 2021 has shown that consumers long for a wider range of telehealth services.
- Lack of telehealth services is one of the top 10 reasons why a patient may be discouraged from booking a visit with a provider.
- The level of investment in telehealth in the first half of 2021 ($14.7 billion) is marginally more than the total amount of investment in 2020 ($14.6 billion).
There are several reasons for this high demand:
Time and cost savings. The ability for patients to access telehealth functionality via a phone or desktop saves time and eliminates the need to take off work and pay for gas, travel, parking, etc. People with tight schedules and those caring for elderly relatives or children often have difficulties visiting a physician in person.
Accessibility. For individuals living in rural areas, it can be hard to access quality healthcare. Transportation issues are even more evident for those who have serious health problems, which makes it challenging to access in-person care.
Privacy and health security benefits. Some individuals might be intimidated or anxious about searching for care related to sensitive health issues. These might include family planning, mental health, and various aspects of women’s and men’s health. Also, people vulnerable to COVID-19, such as seniors and people with underlying medical conditions, are likely to benefit from telehealth.
Telehealth to simplify doctors’ work
In April 2020, Sermo conducted a survey among physicians. They discovered that after the pandemic ends, healthcare specialists are planning to use telehealth technology more often than they used it before. According to McKinsey, 84 percent of physicians (as of April 2021) were consulting via remote healthcare services, and 54 percent intended to keep on with this practice.
Reasons for the demand for telehealth among doctors include:
Improved work–life balance. Doctors want to use telehealth, as it enables a more flexible schedule and helps to reduce burnout. Telehealth functionality helps doctors provide real-time remote services and have greater access to patients. According to a 2019 report by American Well, the specialists that want telehealth most are those with the highest burnout rates. These include specialists in urology, emergency medicine, infectious diseases, neurology, psychiatry, pediatrics, and oncology.
Ability to attract and retain new patients. Doctors consider virtual visits helpful in ensuring convenient, patient-centric care that might widen their patient bases and retain patients. Moreover, by providing timely and easy access to care via virtual visits, doctors think telehealth may improve patient outcomes.
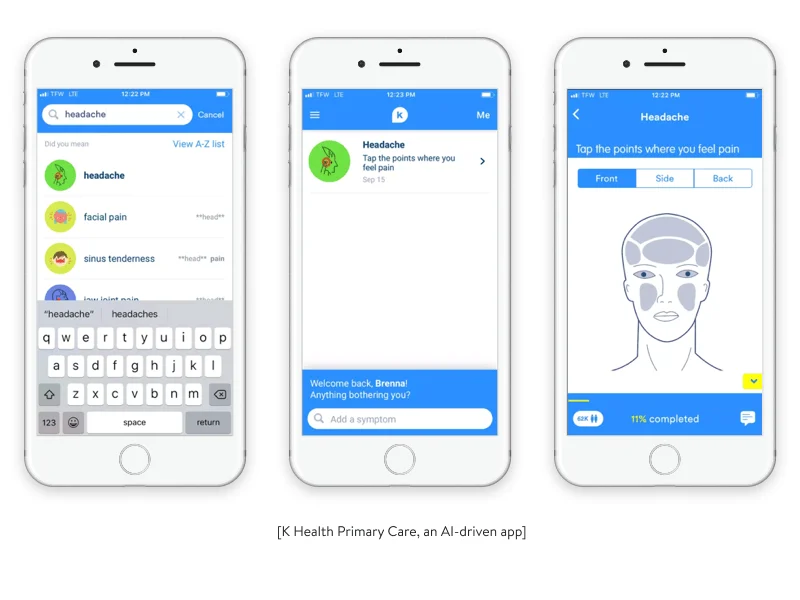
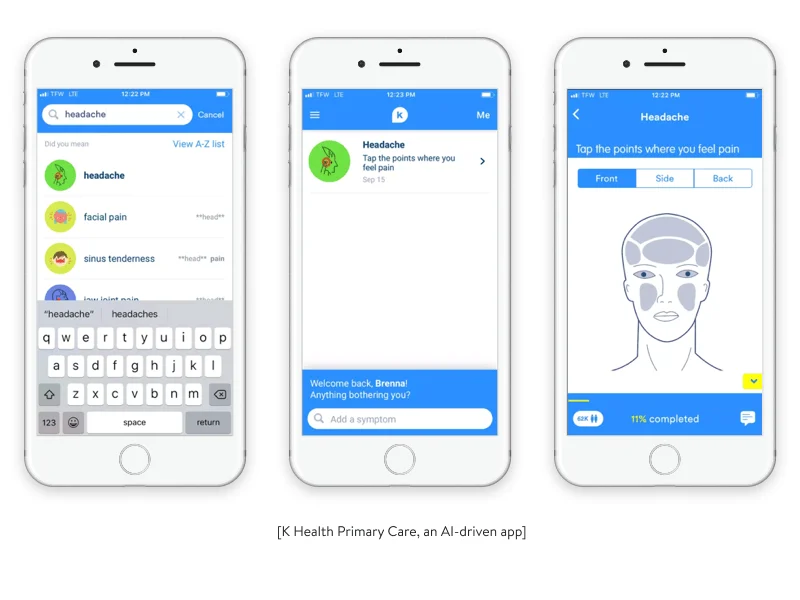
Ability to handle common or minor health issues. According to data by the Association of American Medical Colleges, the US might experience a shortage of 54,100 to 139,000 doctors, including both primary and specialty care physicians, by 2033. Virtual visits might reduce time spent on in-person visits. Telehealth itself and technologies such as artificial intelligence can improve the efficiency of available providers. As a result, doctors can serve more patients faster and ensure that common and minor health issues are solved without their intervention.
The physician shortage is already being acutely felt by medical practices. But telehealth promises them other benefits.
Benefits that telehealth promises for medical practices
Here are some of the most prominent benefits that telehealth offers healthcare organizations.
Fewer costly patient no-shows
Patient no-shows seriously block a practice’s revenue stream. A study by Health Management Technology determined that no-shows cost the US healthcare system $150 billion annually and cost the average doctor $200 per unused time slot. Whether or not a patient shows up, a medical practice still has to pay its workers and cover expenses such as rent and use of equipment.
By delivering remote care to patients wherever they are, providers can not only reduce their no-show expenses but can even increase their revenue, as it’s more convenient for a patient to see a physician virtually. At the same time, providers can fill no-show appointments at the last minute by keeping a waitlist for same-day remote visits.
Reimbursement for telehealth services
Medicare reimburses telehealth services at the same rate as comparable in-person services based on the current Medicare physician fee schedule.
Specialists at distant sites that can get paid for covered telehealth services (subject to state law) include doctors, physicians’ assistants, nurses, nurse midwives, certified nurse anesthetists, clinical psychologists and social workers, nutrition specialists, and registered dietitians.
Most commercial insurers at least partially cover telehealth services, including the largest insurance providers like Aetna, BCBS, Cigna, and United Healthcare. The American Society of Clinical Oncology has compiled a list of many private insurance providers that cover telehealth services along with conditions of coverage provided.
Reduced hospital readmissions
About 82 percent of 3,080 hospitals participating in the hospital readmissions reduction program by Medicare from 2016 to 2019 were penalized for overly high readmission rates according to revcycleintelligence.com.
High hospital readmission rates are a common problem due to the gap between discharge and homecare. During this time, patients can get conflicting instructions and consequently fail to follow their treatment plans.
Telehealth can facilitate treatment outcomes and reduce hospital readmissions while at the same time facilitating the continuity of quality care. This can be ensured through continuous medical education and remote monitoring of a patient’s state of health by tracking vitals after a patient is discharged from the hospital.
Having considered the benefits of telehealth for patients, physicians, and healthcare organizations, let’s touch on the key terms you need to understand before getting down to custom telemedicine app development.
Components of telehealth
When discussing telehealth, we often hear the term telemedicine. Although the terms telehealth and telemedicine are often used interchangeably, they’re not the same.
Telehealth is much broader than telemedicine
Telemedicine is a subset of telehealth, which covers healthcare information, education, and other healthcare services in a broad sense. Telehealth includes helping patients not only directly but also indirectly by assisting, informing, and educating healthcare providers so they can better care for patients.
There are three use cases of telehealth:
Use case 1: To ensure providers’ support and enable collaboration
Tele-ICU (Telemedicine Intensive Care Unit) technology helps off-site clinicians provide bedside staff with e-consulting on patient care. A centralized team of consultants can assist many geographically dispersed facilities in real time and share health data electronically.
Via audio/video calls and a real-time exchange of patient data from several interfaces, a doctor working from a virtual medical center in Los Angeles, for instance, can rapidly care for a patient in Santa Barbara at any time of day. This connectivity allows an intensivist to quickly provide quality care.
Use case 2: To remotely monitor vital signs
Remote monitoring ensures the real-time transmission of data from a patient to a provider. Patients can systematically forward health data including weight, heart rate, pulse, and blood pressure.
Data collection and transmission is typically facilitated by means of Internet of Things (IoT) devices. Wearable IoT devices include the Apple Watch, Fitbit devices, smart touchscreen glucose meters, and implantable cardiac devices. Receiving information from such devices in a timely manner helps a provider promptly adjust treatment and consequently provide better care.
The recent survey by healthinsurance.com that we previously mentioned found that among 1,000 Medicare-eligible seniors that used a telehealth service, 28 percent tracked their vital signs using a wearable device.
And according to the survey cited above by Sermo, among 1,392 doctors, over 90 percent are conducting virtual patient appointments. However, this survey also shows that remote monitoring tools are more widely adopted by doctors in Asia and Europe than those in the US. Only eight percent of US doctors reported using them.These statistics show a low level of wearable device use in the US, despite the benefits wearables may bring in providing high-quality medical services.
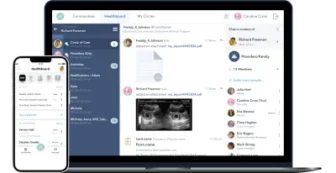
By the way, Healthfully, an all-round healthcare management solution with virtual visit functionality that was created by Yalantis, provides remote patient monitoring tools by means of fitness trackers and medical devices.
Use case 3: To ensure patient engagement via patient portals
Patient portals are secure websites that give patients easy 24/7 access to their personal health data. By logging in with a username and password, a user can check health data such as recent doctor visits, lab results, and medications.
In addition, some patient portals enable patients to schedule non-urgent visits, text their doctors, learn about health-related matters, and even benefit from social community components.
We implemented community components in Healthfully. Medical personnel, relatives, and friends can build a patient-centered community in Healthfully with different levels of access to a patient’s health information. There are also anonymous communities devoted to different health problems in which patients can share their challenges and experiences.
Telemedicine as a component of telehealth
Telemedicine refers specifically to serving patients remotely using telecommunications technology. This includes sharing medical images, remote diagnosis and health assessments, online video consultations, and audio calls.
Video conferences and pre-recorded video guides enable providers to ensure patient-centric assistance for even the most expensive and difficult to treat conditions, including heart disease and diabetes. Paying a virtual visit to patients with these conditions might prevent an unnecessary hospital trip or even save a life.
Synchronous and asynchronous telemedicine
When researching the topic of telemedicine, you might notice mentions of synchronous and asynchronous telemedicine. It’s important to understand how they differ and why implementing both is essential for achieving the goals of your software solution.
Synchronous telemedicine is conducted via video calls.
Asynchronous telemedicine is when a patient transmits medical data to a provider from an offline assessment conducted at a convenient time for the patient. Examples of asynchronous telemedicine are sending still images like X-rays, MRIs, or photos of a skin condition for analysis. Another example of asynchronous telemedicine is when a patient participates in an online doctor-created survey.
Software such as Healthfully allows doctors to conduct surveys to monitor patients’ conditions and satisfaction with care. Setting up trigger parameters in a patient survey in Healthfully allows doctors to receive notifications so they can adjust treatment or suggest extra screenings.
To develop an all-round telehealth solution, you need to make sure you cover synchronous and asynchronous telemedicine functionality. You also need to take into account your healthcare specialization to make sure you meet the needs of your patients and staff.
Telehealth for different healthcare specializations
It’s crucial to understand when telehealth is not sufficient. There are many cases that require detailed examinations (in proctology, dentistry, gynecology, etc.), screenings (fluorographies, gastroscopies, mammographies), and surgeries. Add to that list providing emergency medical care when a patient suffers from loss of consciousness, chest pains, coughing or vomiting blood, or any traumatic injuries.
However, any practice that provides the above-mentioned care can still at least partially use telehealth solutions. For example, pre-operative, post-operative, and other consultations don’t necessarily require in-person visits.
Telehealth works very well for primary, preventive, and chronic care, nutrition, radiology, and less severe yet urgent matters including coughs and colds, migraines, irritable bowel syndrome, erectile dysfunction, allergies, and behavioral health via tele-mental health solutions.
Lots of essential physical exam findings, including rashes or difficulty breathing, might be diagnosed by means of videos or photos. For other examinations, physicians may need extra tools that vary depending on the specialization.
Optometrists may ask patients to take online visual acuity tests and fill out dry eye questionnaires prior to a consultation.
Endocrinologists might use connected glucose meters to automatically upload blood glucose levels to a secure digital account that can provide patients with real-time, personalized suggestions.
Cardiologists might take advantage of the Apple Watch, some versions of which contain an FDA-approved application that can perform and transmit information on EKGs in real time.
It’s vital to consider the specifics of your healthcare domain when you’re planning a real-time telehealth solution.
Basics of how to create a high-quality and secure telehealth solution
Let’s now look at some basic technical peculiarities and tips from our company’s experience developing a telemedicine app.
Telemedicine app and video module architecture
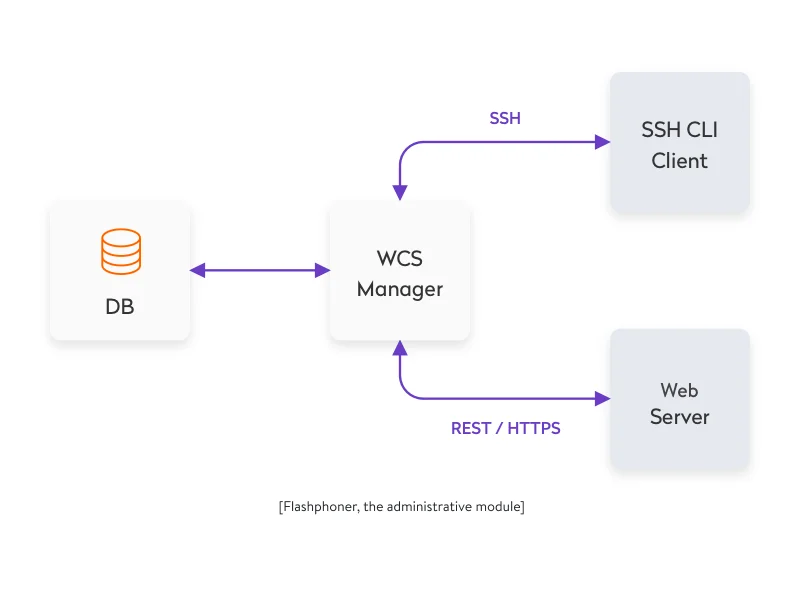
How can you build custom telehealth solutions? Use telecommunications technologies. Start with an out-of-the-box streaming video and audio solution like Flashphoner, TokBox, Ant Media, or Wowza. Each offers its own SDK that provides developers with flexibility to create an app that meets your product requirements.
These ready-made solutions free developers from handling load balancing, traffic prioritization, and lost packages. Moreover, they provide developers with ready-to-use architectures that can be adapted to specific telemedicine software development needs.
Establishing high-quality video and overall security
A secure connection, data storage, and HIPAA compliance are the three pillars of telehealth security. Although US authorities aren’t currently requiring telehealth services to comply with HIPAA, we strongly believe that healthcare solutions must be secure from the outset.
To provide secure patient–provider communication, you need to implement a network security protocol like SSL or TLS. Both help to ensure secure network connections between systems.
What impacts the quality of a video stream? There are multiple factors including how the route between a streaming source and end user is built and how your router is set up. It’s almost impossible for developers to manage such issues. But we can use technologies that allow us to establish an optimized real-time connection.
Peer-to-peer vs client–server networks
There are two approaches to ensuring a video connection. The first is building a client–server network in which video is streamed to a server and then distributed to end users.
This approach is better for pre-recorded videos, as a server can ensure more storage space than most external storage devices attached to a peer-to-peer network. The HLS and MPEG-DASH protocols help to ensure adaptive playback by streaming a video file in parts.
But in order to minimize interruptions during live conferencing, it’s more appropriate to implement a peer-to-peer network, as it provides a better real-time connection. The WebRTC protocol helps to transmit all multimedia communications in real time.
Establishing secure data storage and ensuring HIPAA compliance
To ensure data security, you should keep all passwords and sensitive user data encrypted. Also, use up-to-date security approaches (for example, an SHA hashing algorithm instead of the outdated MD5).
How to ensure HIPAA-compliant video conferencing and data sharing
At Yalantis, our specialists have experience developing HIPAA-compliant software. This is what we did to make Healthfully HIPAA-compliant:
- Followed HL7 standards for sharing medical and administrative data online and ensuring secure and simple storage and data transfers
- Recorded activity logs of all users’ activities to comply with HIPAA (logs must be kept for at least six years) and to enable Healthfully to analyze its processes to increase productivity and improve the customer experience
- Deployed the software on Amazon Web Services to guarantee that all data is encrypted and to allow for building a HIPAA-compliant structure

Additional aspects to consider when creating telehealth solutions
To be able to create healthcare software fast and with high quality, a development team should be well-versed in healthcare industry requirements for e-clinics. Understanding user roles, the needs of each target audience, and technical specifics is a must.
On-premise and cloud-based EHRs, virtual clinics, and other eHealth projects also require lots of integrations, often with legacy systems and poorly documented technologies. It takes developers much time to learn how to use each technology if they aren’t familiar with it and to decide on the best technology stack for a particular project. In some cases, you may need integration with a different EHR system. Yalantis has experience integrating an EHR system with such solutions as Epic, Cerner, Practise Fusion, Nextgen Healthcare, and other systems.
Our business analysts and technical specialists are experienced in all of these things, which helps them choose the most suitable technology stack to develop web and mobile health solutions. If you want to build an on-premise or cloud-based telehealth software solution, we’ll create it for you on short notice. Want to improve your practice’s doctor–patient interactions? We’ll gladly stand by you, providing our outsourcing and outstaffing software development services and sharing our knowledge of how to develop a telemedicine platform.
Remember that the efficient use of high-quality telehealth solutions requires their adequate implementation into an establishment’s workflow and adjustment to the essential needs of your staff and patients. Let’s see how you can wisely satisfy both parties and carry out new practices.
Best practices to implement telemedicine in your clinic or hospital
McKinsey recommends all healthcare stakeholders to “define a value-backed virtual health roadmap.”

Let’s briefly decipher this eight-step telehealth implementation strategy.
1) Identify your need and prioritize your challenges to properly distribute your resources:
- Gather feedback from your frontline staff to spot crucial bottlenecks and opportunities and survey your patients to learn when their satisfaction suffers.
- Align identified issues with your organization’s goals to define which issues you’ll address first.
- Determine if your organization or practice is financially ready for telehealth.
2) Gather your clinical team:
- Outline the team structure.
- Determine where within your organization telehealth will be hosted.
- Distribute responsibilities, set important milestones with exact dates, and then divide your workload by sprints, keeping key objectives in mind.
- Set up weekly updates by email or in a separate chat and set up regular meetings with each team to get control over the implementation process.
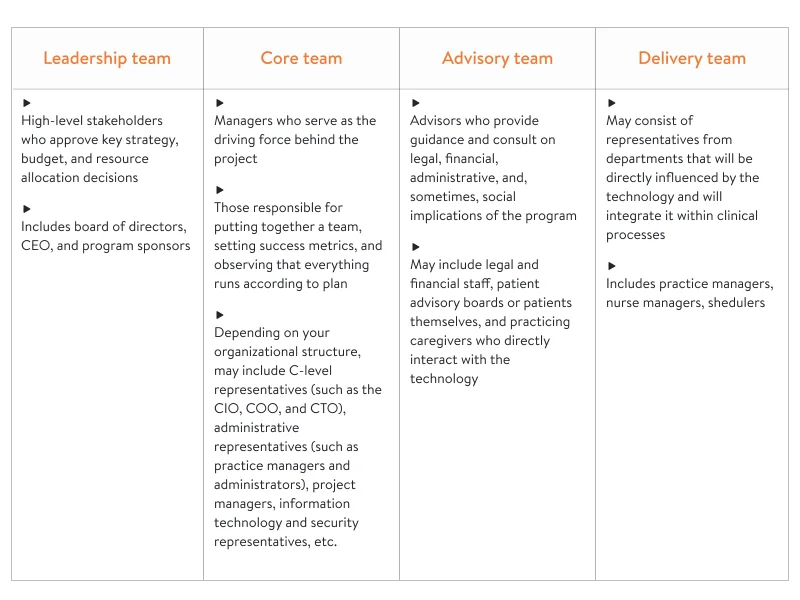
You can also use this chart to understand which team members can be involved and when:
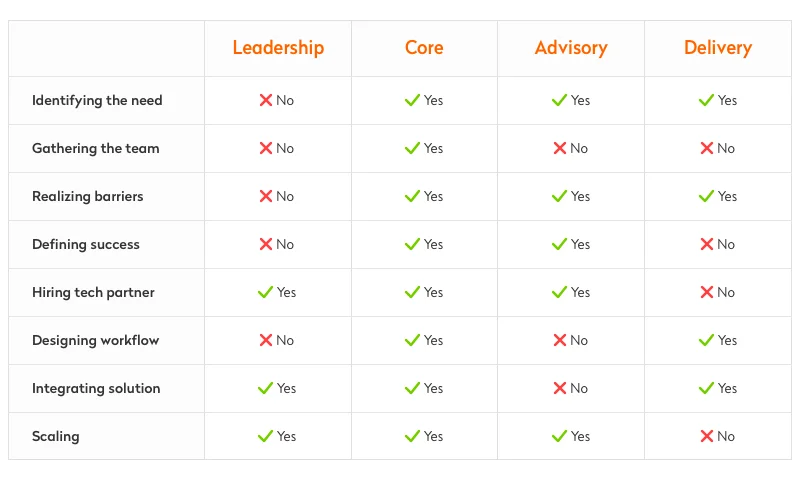
3) Realize barriers: Identify legal, regulatory, financial, social, and technological barriers that could get in your way so you know how to cope with them later.
4) Define success: Set measurable metrics that will help you evaluate if your solution proves effective for your organization.
5) Find and hire a technology partner: Look for a partner whose solution will suit your needs and budget expectations.
There are the four basic criteria to help you narrow down your list of medical software developers:

6) Properly adjust your clinical workflow to the implementation of virtual visits:
- Conduct feedback sessions to find out staff and patient readiness to adopt telehealth services.
- Provide exhaustive support and training materials for your staff and educate your patients on your new offerings.
- Spot where changes will be necessary and work with your delivery team to get their input on the new workflow design.
- Make sure your services are provided legally and adhere to policy and reimbursement requirements.
7) Integrate the solution: Officially launch your telehealth solution to test out your new workflow, from scheduling an appointment to getting through the billing process.
8) Scale: Consider other areas for improvement within your organization (for example, applying telehealth to another department of healthcare delivery network branches).
Yalantis unites with healthcare businesses to help them achieve sustainable growth and optimize business processes through tailor-made digital health technology. If you’re looking for a new opportunity to transform digitally, tell us about your ambition at hello@yalantis.com and we’ll devise an effective way to fulfill it.
Rate this article
5/5.0
based on 1,137 reviews