How to implement health risk assessment functionality in an EHR system
Prevention is better than cure. Today, this proverb is truer than ever. Nowadays, prevention may not only help healthcare consumers avoid pain, risks to life, and heavy spending on treatment but may be much faster and easier than solving health issues when they arise. What has changed in the healthcare industry?
The development of predictive analytics, machine learning services, big data, and other technologies have resulted in health risk assessment (HRA) software. In the past, healthcare providers and patients had to fill out paper forms, which needed to be analyzed and somehow organized by humans, to monitor patients over time.
Today, a health risk assessment might be a matter of several clicks on a phone. The information a patient provides can then be analyzed in seconds based on huge data sets available in an HRA system.
As a result:
- Healthcare consumers can prevent severe consequences of their lifestyles, mitigate genetic predispositions to certain diseases, and minimize the possibility of contracting infections.
- Doctors can spend less time assessing patients and get a more objective view of a patient’s state of health.
- Thanks to huge sets of collected data, medical scientists can effectively analyze trends in an entire population’s health, the spread of infections, etc.
What is HRA software?
An electronic health risk assessment screening solution allows healthcare consumers and providers to define health risks and ensure tracking patients’ health over time. A common HRA tool includes a questionnaire. A self-assessment tool also typically provides personalized advice on actions to take to minimize health risks.
While indicating health risks, however, HRA software can’t diagnose diseases or replace a doctor’s consultation. Still, it might help to:
- prevent serious acquired illnesses including diabetes, hypertension, cancer, and heart disease by identifying predispositions
- reduce the spread of dangerous diseases like COVID-19 by providing resources for counseling and social distancing strategies
- identify the degree of urgency of a medical situation and predict postoperative complications and patient deterioration.
Clinical HRA tools can be roughly divided into three types. The first two are used by healthcare professionals and the last is used by healthcare consumers and is adapted to their needs and perceptions:
- EHR-integrated tools
- Components of clinical decision support (CDS) systems
- Self-assessment tools
Let’s check out the differences between these three types of tools and see how to implement them.
HRA software used by healthcare providers
There are many separate web-based or mHealth HRA calculators that are widely used by hospitals. They might be highly specialized like the OncCOVID app, which enables oncologists to calculate the risk of delayed cancer treatment during the COVID-19 pandemic. There are also apps like Calculate by QxMD, which offers over 400 calculators in different areas including cardiology, nephrology, gastroenterology, oncology, and orthopedics.
But using these tools requires physicians to change screens. Doctors need to leave an EHR to enter patient-specific data in a calculator and go back and forth between an EHR and HRA to find information. Integrating an HRA tool directly into an EHR system is likely to improve the risk assessment process.

EHR-integrated HRA tools
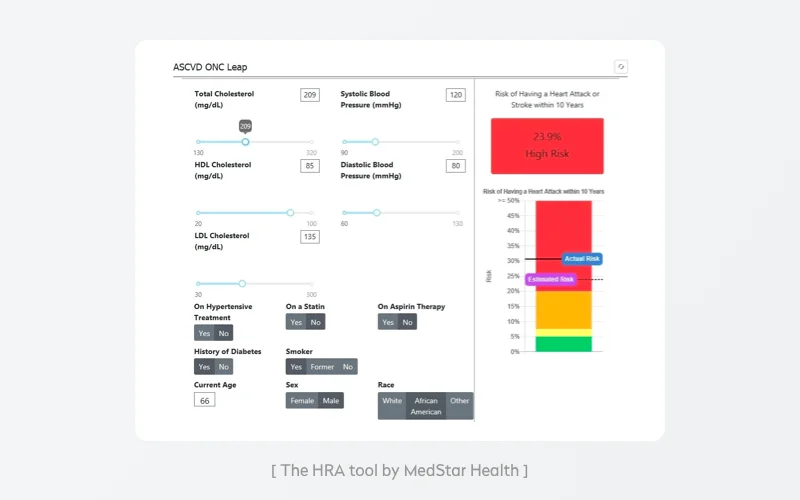
MedStar Health, a Maryland and Washington, D.C.-based health system, wanted to help its cardiologists effectively use the ASCVD risk calculator by the American College of Cardiology. MedStar Health doctors had been actively using the tool, as it’s the gold standard for cardiologists to identify a patient’s 10-year risk of heart-related issues including heart attack and stroke. MedStar incorporated the calculator in a graphical display accessible in their EHR software. To integrate the calculator as a custom component in the EHR, Medstar:
- partnered with the technical team from the American College of Cardiology to ensure proper implementation of the tool
- conducted research to discover how to connect the third-party app with the EHR and how to feed the tool with the most recent data
- used Argonaut interoperability standards and SNOMED codes to ensure smooth and safe medical information exchange
- built the tool as a SMART on FHIR application to ensure a connection with the EHR (we’ll touch upon this subject later in this post).
These steps enabled clinicians to save time and effort while providing the following benefits:
- MedStar’s EHR automatically pre-populates the calculator with patient-related information.
- The calculator became part of doctors’ workflows, indicating risks with no need for doctors to run calculations themselves.
- Doctors can see changes in risk levels over time and take appropriate measures if needed.
- Doctors can easily provide patients with customized lists of advised lifestyle changes, including weight loss suggestions, or point out the urgent need to quit smoking.
You can also go further than creating an HRA tool and build an all-round clinical decision support (CDS) system enhanced with health risk assessment functionality.
CDS system enhanced with HRA functionality
Clinical decision support solutions help doctors detect potential symptoms and manage risk assessments and patients accordingly. They’re usually multifunctional, including alerts and reminders for providers and patients, various documentation templates, and contextually relevant reference information.
Health risk assessment tools are an essential part of a clinical decision support system. Tapa Healthcare, for example, enables its CDS system to observe patients and predict patients’ deterioration. To provide effective HRA functionality, a CDS should be properly integrated within an existing information system, use EHR data, and be based on algorithms.
Integration within existing data systems. A CDS may be a standalone system, but that isn’t the best option. Lots of early CDSs were implemented as systems that required physicians to document or source data outside their main workspace. As a result, the clinician workflow was disrupted. An effective CDS should be a component of a comprehensive EHR system. Healthcare providers should take this into account when implementing EHR systems.
Use of EHR data. An effective CDS should be built upon the foundation of an EHR to pull general and patient-specific data that’s properly filtered and organized. The use of EHR information will enable doctors to detect changes outside their areas of specialization and detect changes specific to particular patients.
Use of algorithms. A CDS tool should be empowered with algorithms for calculating the risk of an individual having an undiagnosed disease or the likelihood of contracting a disease. Ideally, these algorithms should be based not only on symptoms and tests but also take into account such factors as age, gender, and ethnicity. Algorithms should be integrated into a doctor’s general patient management system so they’re available during consultations.
When developing EHR components, whether they be for health risk assessment or any other functionality, focus on fulfilling end user needs.
Let’s now look at HRA functionality from the healthcare consumer’s perspective.
Enabling health consumers to assess their own health risks
EHR-based HRA tools for self-assessment have the potential to ease the workload for doctors, help patients manage their own health, and increase patients’ involvement in healthcare decisions.
MedStar’s EHR-based HRA tool has two important components: patient-facing and provider-facing interfaces. For patients, a risk calculator provides a deep view of their overall health, motivates them to improve their lifestyles, and supports healthy behaviors.
HRA tools for self-use are especially helpful in fighting pandemics like COVID-19, as there’s high demand among patients to check their risk of infection or the possibility of having been infected. Here’s how to provide healthcare consumers with great EHR-based HRA functionality.
Provide user-friendly questionnaires
Risk assessment tools designed for patients often look like boring one-page questionnaires with lots of complicated medical vocabulary. An HRA tool created in this style will almost certainly fail, since an average consumer may provide incorrect information when answering complicated medical questions and won’t come back to retake the questionnaire.
On the contrary, MedStar Health’s heart risk tool provides healthcare consumers with a clear and colorful display of their risk that is understandable and impactful.
Questionnaires provided by your quiz should be user-friendly and designed to elicit essential data from users as quickly as possible. A quiz by Oscar Health estimates a user’s risk of contracting COVID-19, and it takes only about a minute. At the same time, it walks users through all potential risk factors including history of smoking and COVID-19 symptoms like difficulty breathing.
Yalantis took into account the above-mentioned nuances while building a health app concept with a feature for booking doctor’s appointments. To provide doctors with the most vital patient information, we added a brief interactive questionnaire that wasn’t overloaded with text and avoided ambiguous questions.
[Health insurance app concept by Yalantis]
Read also: How to develop a health insurance software solution
Use artificial intelligence to offer a personal approach
To encourage users to keep taking periodic risk assessments, offer engaging follow-ups. Ada, an interactive symptom checker app for iOS and Android, implements an AI-powered system that contributes to personalization. The app’s smart symptom checker enables users to check any symptoms, and the app becomes familiar with a user’s particular conditions and medical history. As a result, the app is able to provide more accurate predictions over time.
You should also consider embedding an intelligent chatbot into your EHR system. Asparia’s intelligent chatbot can be embedded in EHRs to help patients remember their doctor visits, check-ups, and preventive screenings. Asparia interacts with users via text and voice.
Advise users on and guide them through further courses of action
To support healthcare consumers and provide patient safety, ensure relevant suggestions as a result of your assessments. At the end of their COVID-19 quiz, Oscar Health recommends mitigation measures. If one of those measures is to pass inspection for COVID-19, the tool directs the user to a testing center locator to find the closest center and provides suggestions such as calling ahead.
As talking to a physician is another essential part of assessing risks, the survey links smoothly to Oscar’s telehealth solution.
It’s also advisable for HRA tools to provide consumers with health education feedback and recommendations, supporting them in making positive lifestyle changes and preventing disease. When working on the Healthfully enterprise healthcare system, we enabled doctors to remotely engage patients, educate them, and monitor their health statuses.
Healthfully asks users to take customized questionnaires on a daily, weekly, or monthly basis. Each questionnaire covers a set of factors that are most important for the specific patient. If any of these factors change, the patient’s physician gets a notification so they can adjust treatment or recommend extra screenings. Healthfully questionnaires use a simple question and answer style with checkboxes, buttons, dropdowns, and text inputs.
You might need to help patients who require urgent medical attention or longer appointments. These patients also might require more resources (additional time spent by a nurse for care coordination, for instance). A properly implemented risk stratification strategy can help you allocate resources effectively. Let’s see how you can integrate constant risk stratification processes into your practice.
Risk stratification as a way to identify the most vulnerable healthcare consumers
Risk stratification is when patients are systematically categorized according to their state of health and other criteria. This approach helps healthcare institutions manage patients based on their assigned risk levels to effectively allocate limited resources, predict specific needs, and wisely manage a practice’s entire patient roster.
How to perform effective risk stratification
In an article published by the American Academy of Family Physicians, Dr. James Dom Dera, a doctor of family medicine in Akron, Ohio, shares a successful risk stratification approach. When his practice obtained their initial shipment of flu vaccine in 2018, this two-step approach helped them promptly vaccinate the most vulnerable patients. The approach incorporates objective and subjective data:
Step one requires a practice to categorize patients by dividing them into three risk groups — high, medium, and low — based on objective information. This information is taken from payer claims and the practice’s EHR. Objective data might include information about chronic diseases, advanced age, various comorbidities, disabilities, pernicious habits, and a lack of health insurance. If an HRA is built into your EHR system, your EHR can automatically calculate a risk score based on this data. In either case, you’ll need to proceed to step 2 to adjust the score based on extra subjective data.

Step two requires your medical staff to assign all your patients to one of six risk levels based on their professional subjective opinions.
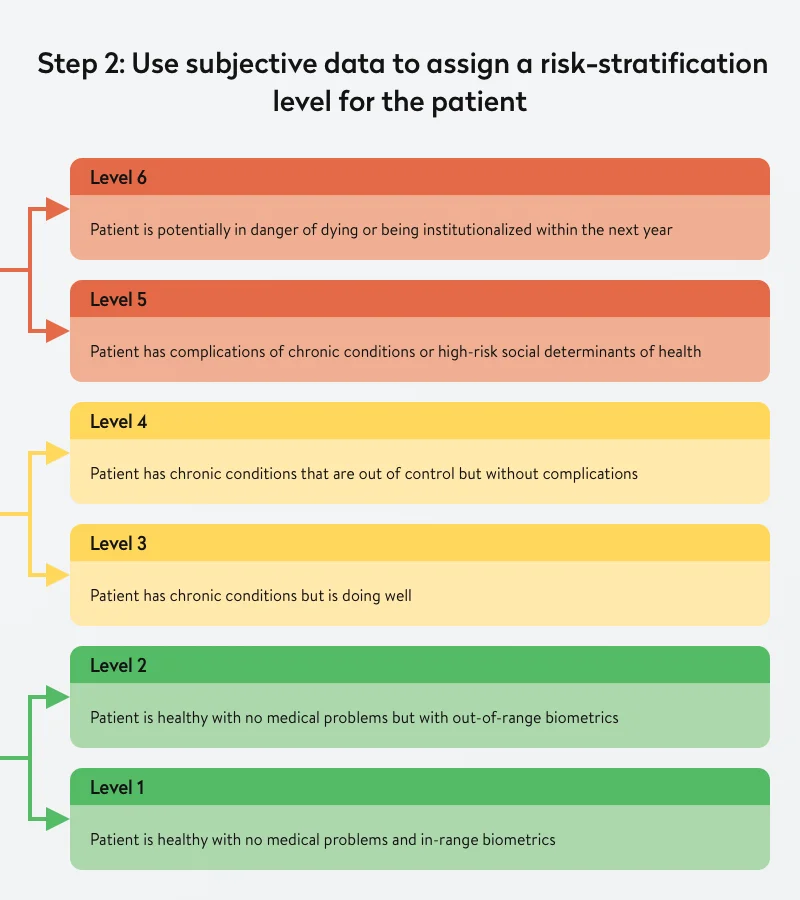
This two-step approach to risk stratification that requires combining objective and subjective data allows the creators of the approach to effectively assess an individual’s risk level.
For instance, say a patient with diabetes has an A1C of 9.2, which classifies them as high risk. But subjective data adds details and indicates that this patient had an A1C of 12 several months ago, which is a more dangerous condition, putting them at risk of kidney failure, stroke, heart attack, and even blindness. Since then, the patient has started exercising and taking medication and has lost 30 pounds. This extra information allows for assigning the patient to a lower risk level.
But what if all this work requiring the time-consuming involvement of medical staff could be automated?
How technology can improve the risk stratification process
You can implement a risk stratification tool as an easy-to-use component of your EHR system. This will enable you to standardize and integrate data from various sources including payer claims, health management systems, and clinical systems. This data might include demographic, diagnostic, and medication data, lab results, and information on current and past symptoms. A risk stratification tool will be able to continuously categorize patients, monitor them, and identify trends.
Paired with medical devices and wearables, such a system can monitor patients’ dynamics. For example, in the case of patients with diabetes, if paired with a blood glucose monitor and fitness tracker, a risk stratification system might show the real-time picture of a patient’s health. This helps doctors accurately assess risk factors to provide the most appropriate care.
Concluding tips on integrating HRA functionality into an EHR system
Creating a web or mobile risk assessment app is challenging. It must be effective and take into account all essential risk factors. The following solutions will help you ensure the quality of your tool.
1. Use specialized tools tailored to your field of medicine
Assessing health risks requires access to statistical data. Often, health risk assessment tools are designed based on medical guidelines from healthcare authorities.
For example, if you wanted to develop a heart disease risk assessment tool for the European market, you could use the SCORE risk charts as a reference. SCORE, which stands for Systemic Coronary Risk Evaluation, is a set of charts that show risk levels based on gender, age, smoking habits, and cholesterol levels.
The American Society of Clinical Oncology provides a digital genetics toolkit that offers oncologists tools and resources to effectively implement hereditary cancer risk assessments.
2. Use third-party APIs
You can choose to build your own symptom checker using APIs of platforms like Infermedica. Infermedica has developed an artificial intelligence-based diagnostic engine that can be integrated into third-party EHRs.
Infermedica’s technology analyzes anonymized patient data in real time and gives clinical recommendations, such as the need to verify symptoms or order lab tests. Behind the API, Infermedica relies on a proprietary statistical knowledge base powered by CDS algorithms created by clinical experts.
Medal, a medical algorithms company, offers thousands of healthcare algorithms by means of APIs. Medal can be integrated with your EMR/EHR system to automatically and anonymously assess patients’ health based on EHR data.
3. Use SMART on FHIR
SMART on FHIR is an open standards-based, interoperable app platform for EHRs. This platform helps EHR systems run third-party apps without the need for costly custom integrations thanks to the adoption of common, interoperable data specifications.
The Fast Healthcare Interoperability Resource (FHIR) is an interoperability specification for exchanging electronic healthcare data. FHIR focuses on providing an easy-to-implement API for healthcare products that’s based on modern web APIs.
The SMART App Launch Framework helps developers connect third-party apps to EHR data, enabling apps to launch from inside or outside an EHR system’s user interface. The framework supports apps for use by healthcare providers, patients, and other stakeholders through any FHIR system. The FHIR standard provides a trustworthy authorization protocol for multiple app architectures, including for apps running on end users’ devices and apps running on secure servers.
You can rely on experienced healthcare software developers to successfully integrate HRA functionality into your EHR system or ensure EHR software implementation or health and safety app development. Yalantis would be a wise choice. We also have experience integrating healthcare solutions with such EHR systems as Epic, Cerner, AdnvancedMD, Athenahealth, and other systems. Our business analysts have deep knowledge of medical practice operations and the technical issues medical practices face. Our developers are experienced in healthcare app development and in building highly integrated, HIPAA-compliant, and complex healthcare systems. We’ll gladly help you automate your clinical processes or even build a custom EHR software system.
Rate this article
4/5.0
based on 75 reviews